Between March 2020 and March 2023, NJ FamilyCare/Medicaid followed special rules related to the federal COVID-19 Public Health Emergency (PHE). These rules allowed members to keep their health coverage, even if they no longer qualified – for example, if their resources were above the allowable limit, which, for most people with IDD, is $2,000.
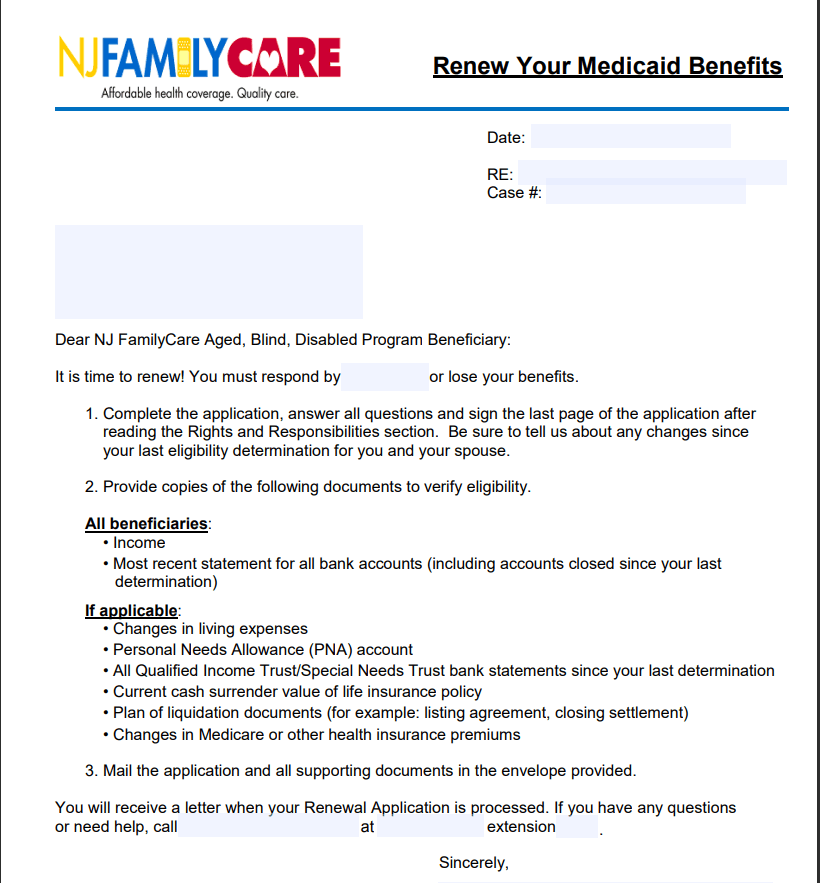
However, Congress passed legislation that requires state Medicaid programs to resume eligibility determinations, as used prior to the pandemic. This process is known as the "Medicaid Unwinding." Since April 2023, Medicaid beneficiaries have been receiving redeterminations, and many beneficiaries will now renew their Medicaid coverage on an annual basis.
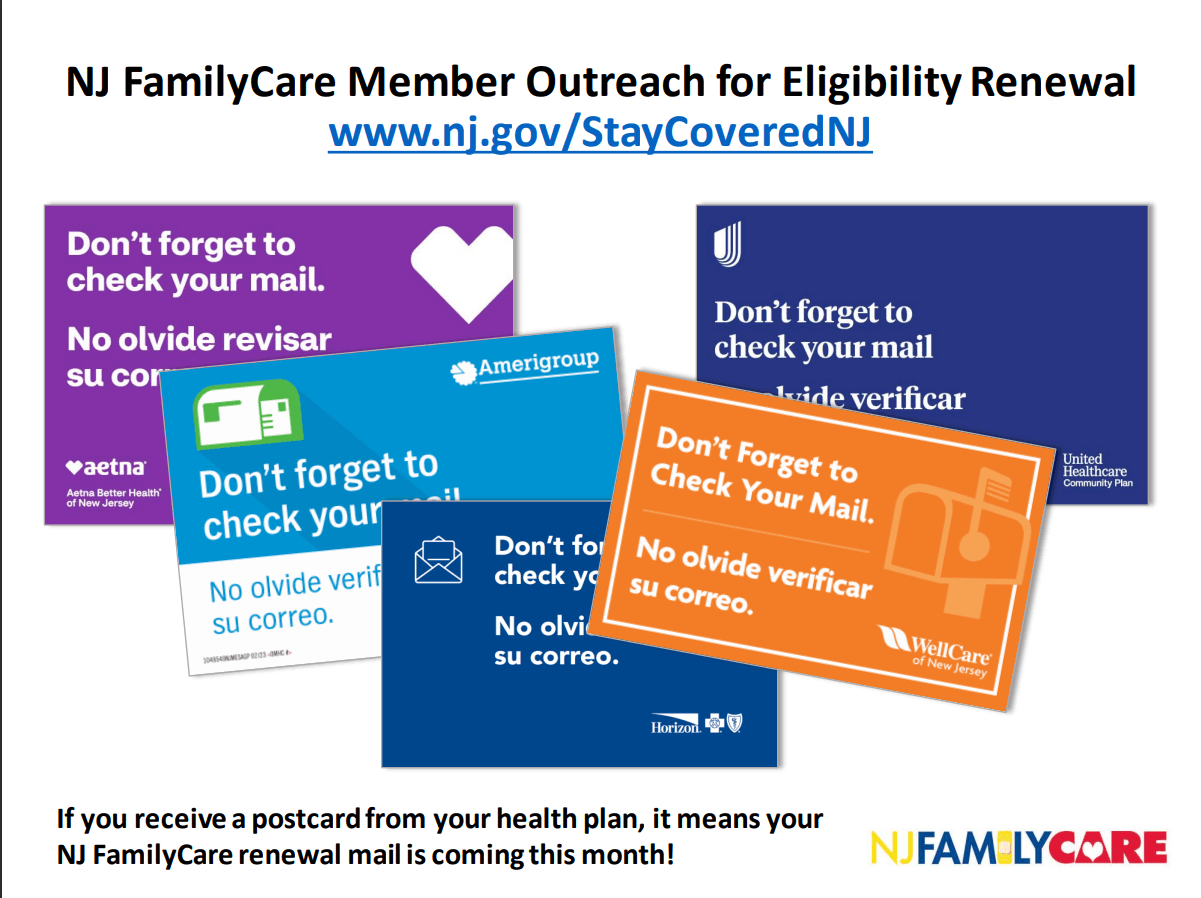
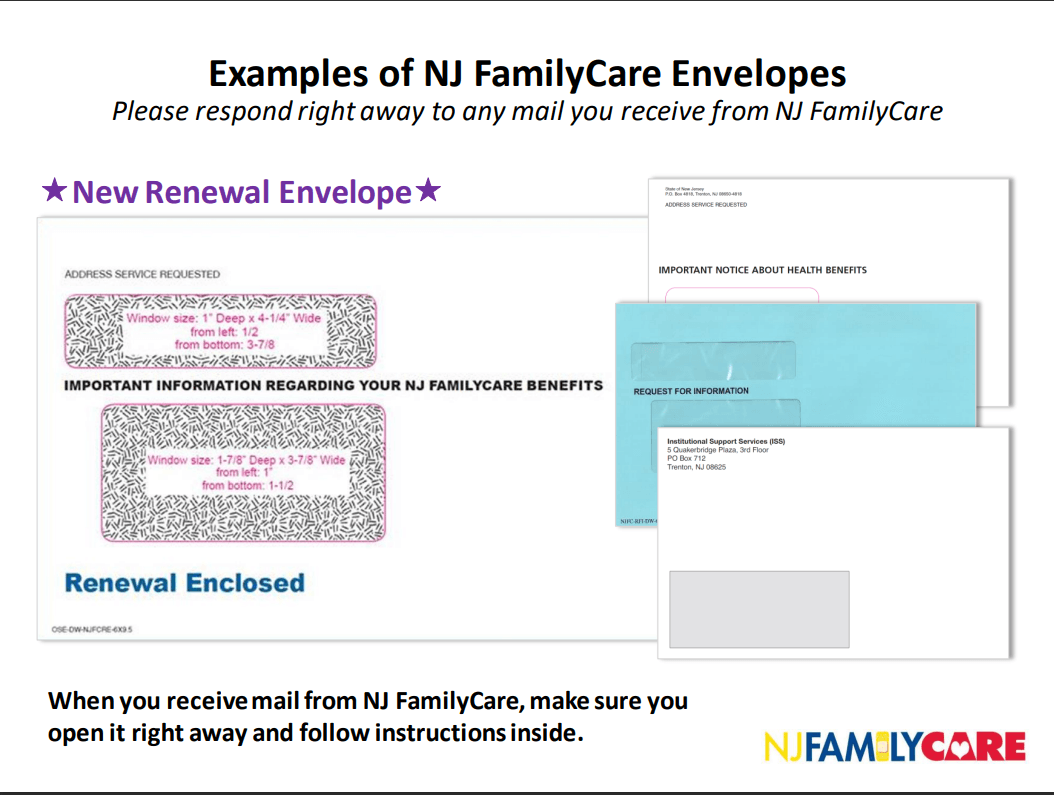
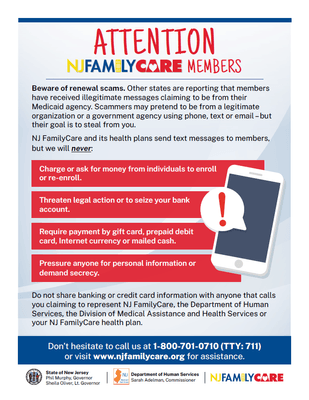
As part of this redetermination, many members will receive mail from the State of New Jersey or their County Board of Social Services. Members will have to provide or confirm additional information so that NJ FamilyCare/Medicaid can decide whether they still qualify for healthcare coverage. Members who do not respond to NJ FamilyCare/Medicaid mail may lose their coverage.
Renewal Information
Every person with IDD who has DDD services must have NJ FamilyCare/Medicaid. People with IDD who receive NJ FamilyCare/Medicaid are required to have a "redetermination" of their Medicaid eligibility. The exception to this requirement is people who receive Supplemental Security Income (SSI).